Jay Iyer ’25, a Molecular & Cellular Biology and Statistics dual concentrator, is on a quest to study rare neurological disorders. He spent a summer interning at three hospitals across India, where he explored the state of healthcare and worked to pitch a new iPad application that uses machine-learning to aid in the diagnosis of neurological disorders like Parkinson’s disease. He shares his own familial experience with rare brain disease, which fuels his passion for further innovation.
“When I was six years old, I learned that my maternal cousin had a rare neurological disease known as Neurodegeneration with brain iron accumulation (NBIA). This is a rare, inherited movement disorder characterized by an abnormal accumulation of iron in the brain, and eventual degeneration of the nervous system1. Her disease variant is so rare that only one other person in the world has it. Over time, my cousin was unable to move without assistance, let alone complete daily tasks. This prompted frequent visits to Connecticut, where I was able to see the effects of this devastating disease firsthand, and help out in any way that I could. Being aware of the dementia that is highly prevalent in my family, I began to wonder ‘Why is brain disease so prevalent in my family?’
Back at home in Baton Rouge, Louisiana, I spent most of time when I was not in school in the garden with my grandfather, Thatha. My small hands were carefully guided by his as we took care of our backyard garden filled with Indian spice plants. To satisfy my endless curiosity, we began to perform little experiments in our backyard, such as watering our spice plants with Coca-Cola and Capri Sun and testing which type of fertilizer would cause them to grow the tallest. Often, due to my lack of scientific understanding, these rudimentary experiments would fail, or the conclusions I drew would be incorrect. Regardless, I continued to learn and fuel my scientific interest with every experiment I conducted.
![Headshot - Jay Iyer[23] copy](https://mittalsouthasiainstitute.harvard.edu/wp-content/uploads/2023/04/Headshot-Jay-Iyer23-copy.png)
Jay Iyer ’25.
Another rare movement disorder known as Progressive supranuclear palsy (PSP), an atypical parkinsonism, found Thatha in 2016, and he was unable to work in the garden with me any longer. Soon, our beautiful garden began to wilt. While I took care of Thatha—from feeding him to holding him as he walked—over the course of three years, I longed to find a way to relieve his pain. I began to look into treatments for his illness, without any success. My frustration became the source of my motivation to better understand the complexity of the brain and the lack of treatments for his disorder. His PSP was more complex than I had ever imagined, and as there are other families struggling with losing a loved one to such an illness, I founded a nonprofit organization and now Harvard student organization, known as Mani Iyer Neurodegenerative Diseases (MIND) Relief, which provides support to patients and families with PSP, CBD, and MSA.

Jay with his grandfather, who suffered from Progressive supranuclear palsy, an atypical parkinsonism.
Today as a sophomore at Harvard College concentrating in Molecular and Cellular Biology + Statistics, with a secondary in Global Health and Health Policy, I aim to leverage wetlab and computational techniques to unlock the secrets of rare brain disease. I believe that by learning how the brain is built, one can learn how the brain can degenerate, and discover specific mechanisms that can be targeted to “shield” the brain from degeneration over time. Thus, I work in the Macklis Lab on campus, studying cortical development in mice. I apply my statistics knowledge in analyzing clinical trial datasets for Parkinson’s disease (PD) and PSP with physicians and statisticians at MGH. I have also written encylopedia chapters and are conducting studies on the relationship between dementia, movement disorders, and sleep.
When my family first suspected that my grandfather may have a movement disorder, we immediately took him to a neurologist, who diagnosed him with Parkinson’s disease. However, this was the incorrect diagnosis, and it took visits to four other neurologists before the correct diagnosis was made. In fact, the rate of misdiagnosis of PD is estimated to be approximately 20 percent2. This is owing to the fact that diagnosing movement disorders is inherently subjective, as it relies on a physician “rating” the severity of certain movements in a battery of tests. As a result, one of my research interests have been to leverage computational techniques to provide an objective metrics for the severity of a movement such as a tremor.
I was lucky when I found the Harvard Undergraduate Global Alliance for Medical Innovation (GAMI), a student-run nonprofit organization that develops medical technologies for use in under-resourced settings. They had a project involving an iPad application and analysis pipeline that extracted features from hand-drawings to diagnose PD. Since joining the project in Fall of 2021, we have begun clinical trials at the Beth Israel Deaconess Medical Center, and are making strides in machine-learning guided diagnosis of PD. However, the question from my childhood still lingered in me, as I continued to wonder why my family has had such an atypical prevalence of rare brain disease, specifically movement disorders and dementia. Are people from Indian descent more likely to develop these types of neurological disorders? I also thought that that the development of a point-of-care diagnostic platform for these diseases may prove to be extremely valuable for clinics in India.
With funding from GAMI and the SEAS department at Harvard, I set out to India in January of 2023 with the intentions of (1) Learning more about the current state of neurological healthcare in India, with an emphasis on movement disorders, and (2) Pitching our iPad application and analysis pipeline to them to determine whether they could test the device for us, and if it would be useful to them in a clinical setting to aid in diagnoses. Through clinical contacts and collaborations in the US, I had identified three hospitals in India that I would visit: NIMS Hyderabad; KIMS Hospital Hyderabad; and Manipal Hospitals Bangalore.

Jay on the second floor (Neurology and Neurosurgery unit) at Manipal Hospitals, Bangalore.
When I visited Nizam’s Institute of Medical Sciences (NIMS), a public hospital in Hyderabad, I was initially taken aback when I saw the sheer amount of people that were sitting in the neurological ward. After speaking to a physician there, she mentioned how she regularly sees 50-60 patients a day, and how it is difficult for everyone to get the required tests, such as imaging, that is easily obtained in the U.S. She emphasized how important a computational-based diagnostic tool could be in helping in making diagnoses. Naturally, it is difficult for a human to make 100% accurate diagnoses in subtle diseases by judging motor function alone. Due to KIMS and Manipal being private hospitals, I noticed that there were less patients being seen per day, but still more than in the United States. All three sites were willing to serve as clinical testing centers for our application and analysis pipeline for the screening of movement disorders.
I carefully shadowed a movement disorders specialist, Dr. Prashanth LK, at Manipal Hospital in Bangalore, India for about a week. Over the course of the week, I got caught up with the current research projects in PD and PSP in India. In comparison to the United States, where a physician may see 1-2 PSP patients a day, I was able to see 6-7 PSP patients each day. Furthermore, I learned that they were able to recruit 300 PSP patients for a genome-wide association study (GWAS) in just one year, in contrast to 5-10 years in the US. Therefore, the increased prevalence of PSP and PD in those with Indian descent may be a real thing, but the question that still remains unknown is whether this is a function of the higher population in India, or if this is due to genetics. We hope that some answers will be found at the conclusion of the GWAS that I will be a part of after participants complete the trial.

Jay and Dr. Prashanth LK, a renowned movement disorders specialist in Bangalore, India.

Jay and Dr. Prashanth LK have a traditional Karnataka lunch.
During that week, I learned a lot about the current state of neurological care in India, and their way of gaining information from the patient in subtle ways to aid in differential diagnosis. In India, it is taboo to speak about many things that may be commonplace to talk about in the U.S. Dr. Prashanth was very clever in his decisions to ask certain questions to gain insight into the patient’s medical history. One of the other things I helped with during that week is to create easy-to-read, digestible pamphlets on Parkinson’s disease and PSP, so that the patient can take these materials home to read in order to learn more about the disease. I also spoke with patients and families suffering from PD, PSP, and related disorders, and worked with them to understand their support needs. Finally, I trained the clinical research coordinators at the hospital on how to collect drawing data using our tablet. I aim to continue working with Dr. Prashanth LK on several research projects beyond the clinical trial of our application, including discovering PSP risk gene variants in the Indian population, and their relation to those already described for the European/US population, as well as other review articles.
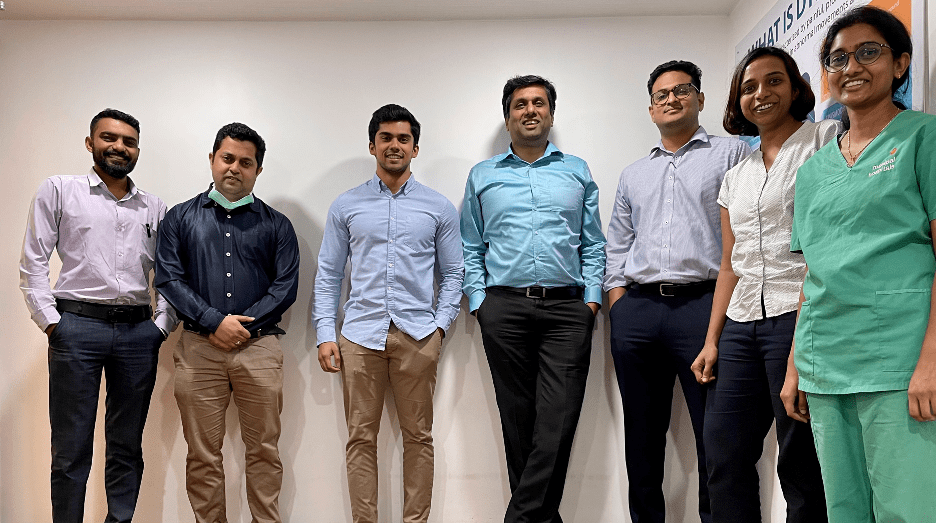
Manipal Hospital in Bangalore group photo, left to right: Dev Sreenivasa (clinical trials specialist); a neurosurgeon; Jay Iyer; Dr. Prashanth LK; Dr. Viksheeth Shetty (neurosurgeon); a neurologist; and an intern.
After the conclusion of our clinical trials in the U.S and India, and pending validation of our tablet-based screening platform, we aim to apply for FDA approval. We hope to implement this technology in hospitals across the US and provide it to low-income areas across the world at a lower cost or for free. Professionally, I hope to become a physician-scientist focused on developing treatments for rare neurological diseases such as PSP.
